Intern Ultrasound of the Month: Hydronephrosis
The Case
70-year-old male with past medical history including severe ureteral stenosis requiring bilateral nephrostomy tubes and ureteral stents who presented to the emergency department for fatigue, chills, and decreased oral intake. He reported that he still urinates spontaneously, though his recent output has decreased. His vital signs were stable, and he was alert and mentating appropriately. On exam, he did not have any abdominal or costovertebral angle tenderness. His nephrostomy tubes were in place and draining non-bloody urine.
Given his complex urologic history, a broad workup was initiated, including labs, urinalysis, and CT abdomen/pelvis. While waiting for results, a renal point-of-care ultrasound (POCUS) was performed to quickly assess for any evidence of hydronephrosis.
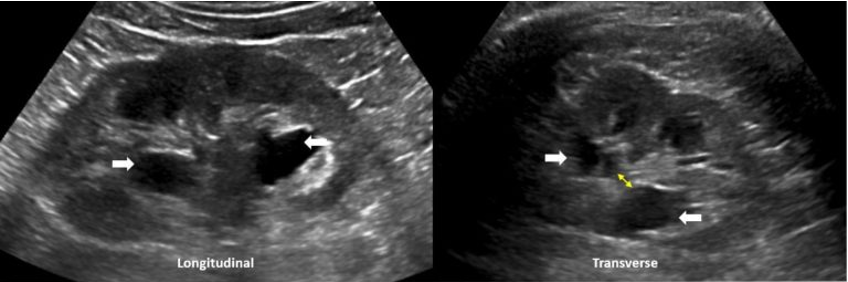
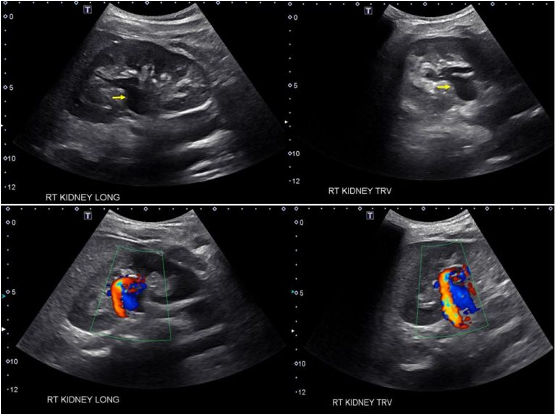
POCUS findings:
Dilated renal pelvis with multiple coalescing, anechoic calyces and parenchymal thinning, consistent with severe hydronephrosis bilaterally — new on the left, with more cortical thinning noted on the right. The bladder (not shown here) was fully decompressed.
A Review of Renal POCUS
Key Clinical Questions: Is hydronephrosis present? Is there urinary retention?
Anatomy of the kidney
Understanding normal renal anatomy is essential before interpreting pathology on ultrasound. A normal kidney typically demonstrates: a hyperechoic renal sinus (central area), hypoechoic or isoechoic renal cortex, and well-defined corticomedullary differentiation [1].
Figure 1. Sonographic Anatomy of the Kidney [1].
How to Perform the Exam
Patient Positioning: Supine.
Transducer: Curvilinear probe (2–5 MHz) is ideal.
Right Kidney
Longitudinal: Place the probe in the right mid-axillary line between the 10th-11th intercostal space, with the indicator toward the patient’s head. Rotate slightly counterclockwise to try to avoid rib shadows.
Transverse: Rotate the probe 90° counterclockwise from the longitudinal view so the indicator points posteriorly.
Left Kidney
Longitudinal: Place the probe in the left posterior axillary line between the 8th-10th intercostal space. Because the left kidney lies more superior/posterior, your knuckles should be touching the bed.
Transverse: Rotate 90° counterclockwise from longitudinal so the indicator points anteriorly [1,2].
Bladder
Always include a bladder view for a complete renal ultrasound exam. Place the probe in a the suprapubic region in sagittal and transverse planes (indicator toward the patient’s head and right, respectively), and fan through the entire structure [3,4]. This allows assessment for urinary retention (i.e. large post-void volume) and identification of causes of hydronephrosis, such as bladder outlet obstruction, stones, clot burden, or mass effect [3].
Hydronephrosis
Definition: Hydronephrosis is dilation of the renal pelvis and calyces due to more distal obstruction of urine outflow [3].
Pathophysiology: Obstruction → increased hydrostatic pressure in the collecting system → increased intraglomerular pressure → decreased GFR [3].
Causes: Ureteral or bladder stones, benign prostatic hyperplasia (BPH), neoplasm (bladder, renal, pelvic), aneurysms (e.g., AAA), pregnancy (especially with a full bladder) [3].
Hydronephrosis Grading:
Grade 1: Dilatation of the renal pelvis only
Grade 2: Dilatation of the renal pelvis and major calyces
Grade 3: Dilatation of the renal pelvis, major and minor calyces
Grade 4: Dilatation of the entire collecting system (i.e. renal pelvis, major and minor calyces), with thinning of the renal parenchyma [3].
**Both of this patient’s kidneys appear to have grade 4 or severe hydronephrosis based on ultrasound.
FIgure 2. Hydronephrosis Grading [1].
Hydronephrosis mimics:
Extrarenal pelvis: Anechoic area adjacent to the renal sinus without calyceal dilatation or cortical thinning (which are seen with hydronephrosis) [5].
Figure 3. Extrarenal Pelvis on Ultrasound [5].
Parapelvic cysts: Cystic masses in the renal sinus. They are non-communicating unlike hydronephrosis where calyces communicate [6].
Figure 4. Parapelvic Cysts [6].
Prominent renal vasculature: Anechoic central regions may mimic hydronephrosis. Apply color doppler to differentiate — vessels will show flow [6].
Figure 5. Vascular Malformation [6].
Clinical Significance of Renal POCUS
Renal POCUS is a great rapid bedside tool for evaluating urinary tract pathology, especially hydronephrosis and urinary retention [7,8]. It can reduce CT utilization, limiting contrast and radiation exposure [7].
A meta-analysis found that in acute kidney injury, POCUS had a sensitivity of 85% (CI 71-94%) and specificity of 78% (CI 68-87%) for diagnosing hydronephrosis [9].
While outside the scope of the emergency department, POCUS can also guide procedures such as renal biopsies or percutaneous drainage, enhancing safety and minimizing radiation exposure [10].
Case Conclusion
Labs revealed acute kidney injury. CT confirmed severe bilateral hydroureteronephrosis with displacement of the left ureteral stent. Urology and Interventional Radiology were consulted, and the patient was admitted to medicine for further management.
Take Home Points
POCUS is a rapid, safe, and effective first-line imaging tool for evaluating for hydronephrosis.
POCUS can reliably detect hydronephrosis (as well as urinary retention), differentiate it from mimics, and expedite care.
Accurate interpretation requires proper scanning technique and knowledge of renal anatomy.
Hydronephrosis appears as an anechoic area within the renal collecting system, starting centrally and expanding outward with increasing severity.
Always include a bladder view: a full bladder suggests outlet obstruction, while a decompressed bladder points to an upstream cause.
AUTHORED BY: NICOLE MINNERATH, DO
FACULTY CO-AUTHOR/EDITOR: LAUREN MCCAFFERTY, MD
References
Deschamps J, Dinh V. Renal Ultrasound Made Easy: Step-by-Step Guide. POCUS 101. Published 2023. Accessed September 24, 2024. Available from: https://www.pocus101.com/renal-ultrasound-made-easy-step-by-step-guide/.
Noble VE, Nelson BP. Manual of Emergency and Critical Care Ultrasound. 2nd ed. Cambridge, UK: Cambridge University Press; 2011.
Soni N, Hariri R. Ultrasound of the Kidneys and Urinary Tract. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563217/.
University of Chicago Medicine. Renal ultrasound. Vimeo. Published 2013. Accessed September 24, 2024. Available from: https://vimeo.com/69556457.
García-Pérez A, Romero-Fresnedo M, Morales-Ruiz M, et al. The Role of Ultrasound in the Evaluation of Renal Pathology: An Overview. J Clin Med. 2017;6(10):87. doi:10.3390/jcm6100087. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5628238/.
Renal Fellow. The Ultrasound Mimics of Hydronephrosis. Renal Fellow Network. May 10, 2019. Accessed September 24, 2024. https://www.renalfellow.org/2019/05/10/the-ultrasound-mimics-of-hydronephrosis/
Harris B, Lentz K, Bell E, et al. Ultrasound in the Diagnosis of Kidney Disease: A Review. Am J Kidney Dis. 2020;76(6):857-867.
Moore CL, Daniels B, Singh D, et al. Prevalence and clinical importance of non-diagnostic point-of-care renal ultrasound. Acad Emerg Med. 2016;23(4):468-476.
Zarifian A, Tabrizi R, Arshadi H, et al. The role of point-of-care ultrasound in detecting hydronephrosis: A systematic review and meta-analysis. Ultrasound. 2023;11(1):1-11.
Rao R, Gubbi S, Shivakumar V, et al. Role of Point-of-Care Ultrasound in Evaluating Acute Renal Failure: A Systematic Review. Ultrasound Q. 2021;37(3):237-245. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8377938/.