Intern Ultrasound of the Month: POCUS & Regional Wall Motion Abnormalities
The Case
70-year-old female with PMH including hypertension and diabetes who presented to the emergency department via EMS s/p witnessed PEA arrest. She initially called 911 for chest pain, shortness of breath, and generalized weakness, and EMS found her to be hypotensive and bradycardic. She subsequently arrested, and ROSC was achieved after 2 minutes of CPR. She was profoundly bradycardic so EMS initiated transcutaneous pacing at rate of 80. Her mentation improved en route.
On arrival to the ED she was alert and conversant. Denied chest pain or other symptoms. Bradycardic on the monitor. While the team was transitioning her to the ED monitor and placing EKG leads, cardiac POCUS was immediately performed and revealed the following:
POCUS findings: Variation in rate between the different views. LV function is reduced, and there is anterior hypokinesis, best seen on the parasternal short axis view. A small pericardial effusion without signs of tamponade is also present; there’s systolic, but not diastolic, RV collapse and no atrial collapse. Findings are concerning for anterior ischemia with insufficient mechanical capture.
Case continued: EKG obtained shortly after confirmed POCUS suspicions, showing an anterolateral STEMI with reciprocal depressions, along with 3rd degree heart block. A STEMI alert was paged. The patient received aspirin, brilinta, heparin bolus. She continued to be bradycardic, and despite lack of electrical and mechanical capture with pacing, she remained relatively hemodynamically stable and mentating well. She received glucagon for possible component of beta blocker toxicity and was also started on an epi drip when vitals declined slightly. She stabilized prior to leaving the ED. Transvenous pacing was deferred as she was immediately taken up to the cath lab where she underwent LAD PCI. She ultimately required impella placement, and the family decided to transition to comfort care.
POCUS & Regional Wall Motion Abnormalities (RWMA)
Brief Background
Coronary artery disease is the most common form of heart disease and is the leading cause of death in the U.S. [1]. Comprehensive echo has a well-established role in evaluating for regional variations in function [2], while point-of-care ultrasound, such as by emergency physicians, has generally aimed to assess global function, pericardial effusion, and right heart enlargement. More recently, emergency physician-performed POCUS has demonstrated diagnostic utility in the evaluation for acute coronary syndrome (ACS) [3-4].
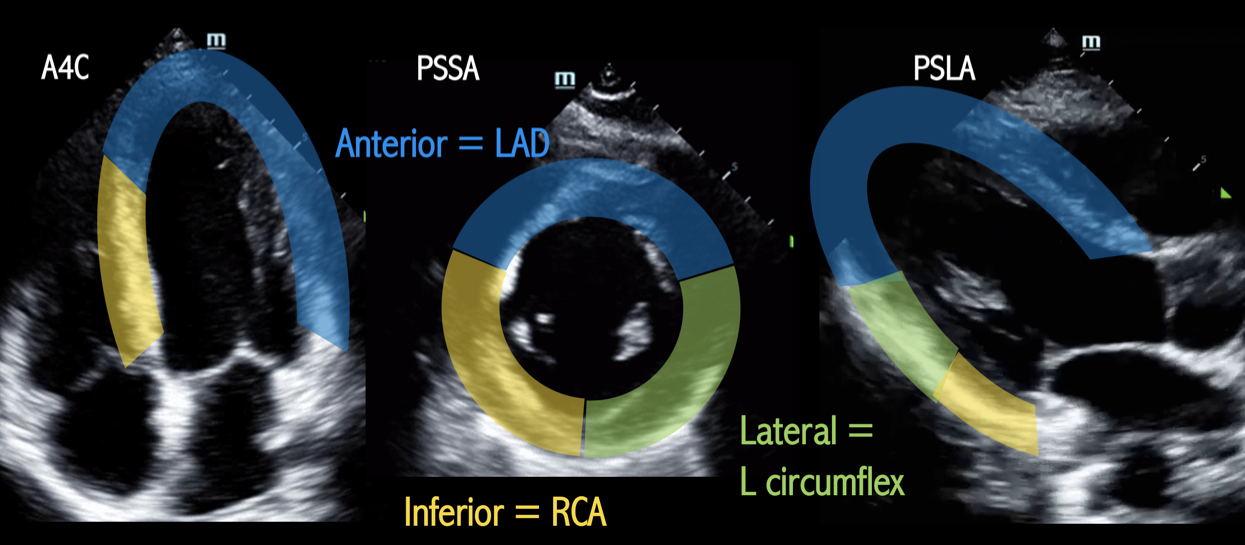
Anatomy - Three Segment Assessment
Simplified version of the AHA’s proposed 17 segment quantitative assessment [5-6].
LV segment correlation with coronary artery perfusion territories
Anterior wall = Left anterior descending artery (LAD)
Inferior wall = Right coronary artery (RCA)
Lateral wall = Left circumflex (L Cx)
What is considered RWMA?
Hypokinesis, dyskinesis, akinesis of one (or more) LV segment(s) compared to the rest of the LV
That particular ventricular wall segment may have asymmetric contractility or myocardial thinning
How to evaluate for RWMA?
Obtain multiple cardiac views; the more the better. However, the parasternal short axis view at the level of the papillary muscles is often preferred as it allows for the best simultaneous visualization of the different walls.
*If too basilar or too apical, or if slightly off-axis, the assessment may appear falsely normal or abnormal.
Assess qualitatively for abnormal LV wall segment contractility/thinning based on the 3-segment assessment above
Potential Pitfalls
Patient anatomy, body habitus, pulmonary disease, positioning
Off-axis views can lead to false positive or negative assessments
Pre-existing or concurrent pathology —>Like with EKGs, it’s always helpful to compare to a previous echo [7].
What Does the Evidence Show?
RWMA are one of the earlier clinical signs of coronary ischemia, often preceding EKG changes and acute thrombotic events. When combined with history and clinical findings, RWMA assessment with echo is thought to improves diagnostic ability and helps with risk stratification for ACS [8].
RWMA are highly associated with acute myocardial infarction and predictive of in-hospital complications, more than the more conventional methods [9].
Emergency physicians can quickly identify RWMA correlating with significant coronary ischemia [3] with fairly high diagnostic accuracy (sensitivity 88%, specificity 92%) as well as localization of RWMA with STEMI [4].
Take Home Points
POCUS is effective in the evaluation of ACS and helps with risk stratification. Correlate POCUS findings with EKG findings as well as prior echos.
While its absence doesn’t rule rule out ACS, the presence of RMWA can help expedite additional workup and definitive management.
POCUS can recognize ACS earlier than conventional testing and, therefore, may be particularly useful when the presentation and/or traditional workup are nondiagnostic.
Additionally, POCUS is useful (in the post-ROSC phase or otherwise) in narrowing the differential for hemodynamic instability. *A whole other topic but worth noting here :)
AUTHORED BY: DR. DANIEL SAADEH, PGY1
FACULTY CO-AUTHOR/EDITOR : DR. LAUREN MCCAFFERTY
References
Centers for Disease Control and Prevention: Heart dis- ease facts & statistics. cdc.gov. https://www.cdc.gov/ heartdisease/facts.htm. Accessed April 22, 2021.
Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines of the Clinical Application of Echocardiography). Circulation. 2003;108(9):1146–62.
Frenkel O, Riguzzi C, Nagdev A. Identification of high-risk patients with acute coronary syndrome using point-of-care echocardiography in the ED. Am J Emerg Med. 2014;32:670-672.
Croft PE, Strout TD, Kring RM, Director L, Vasaiwala SC, Mackenzie DC. WAMAMI: emergency physicians can accurately identify wall motion abnormalities in acute myocardial infarction. Am J Emerg Med. 2019; 37(12):2224-2228.
Cerqueira M, Weissman N, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart A statement for healthcare professionals from the cardiac imaging committee of the council on clinical cardiology of the american heart association Circulation. 2002;539-542.
Johnson B, Lovallo E, Frenkel O, Nagdev A. Detect cardiac regional wall motion abnormalities by point-of-care echocardiography. https://www.acepnow.com/article/detect-cardiac-regional-wall-motion-abnormalities-point-care-echocardiography/. Accessed 4/22/2021.
Ma OJ, Mateer JR, Reardon RF, & Joing S. (2014). Ma and Mateer's Emergency Ultrasound. New York, NY: McGraw-Hill Education.
Ha, E. T., Cohen, M., Fields, P. J., Daele, J. V., & Gaeta, T. J. (2019). The Utility of Echocardiography for Non-ST-Segment Elevation Myocardial Infarction: A Retrospective Study. Journal of Diagnostic Medical Sonography, 36(2), 121-129
Sabia P, Afrookteh A, Touchstone D, Keller M, Esquivel L, Kaul S. Value of regional wall motion abnormality in the emergency room diagnosis of acute myocardial infarction A Prospective study using two-dimensional echocardiography Circulation. 1991;84:85-92.