Intern Ultrasound of the Month: Acute Cholecystitis
The Case
30yo female with PMH significant for obesity s/p prior bariatric surgery presented to the emergency department for progressively worsening RUQ pain, nausea, and vomiting since the evening prior. Also reported right flank pain described as a "pulled muscle."
On exam, her vitals were stable. Her exam was significant for moderate RUQ tenderness with positive Murphy’s sign, no signs of peritonitis. Also had mild right CVA tenderness.
Biliary POCUS revealed the following:
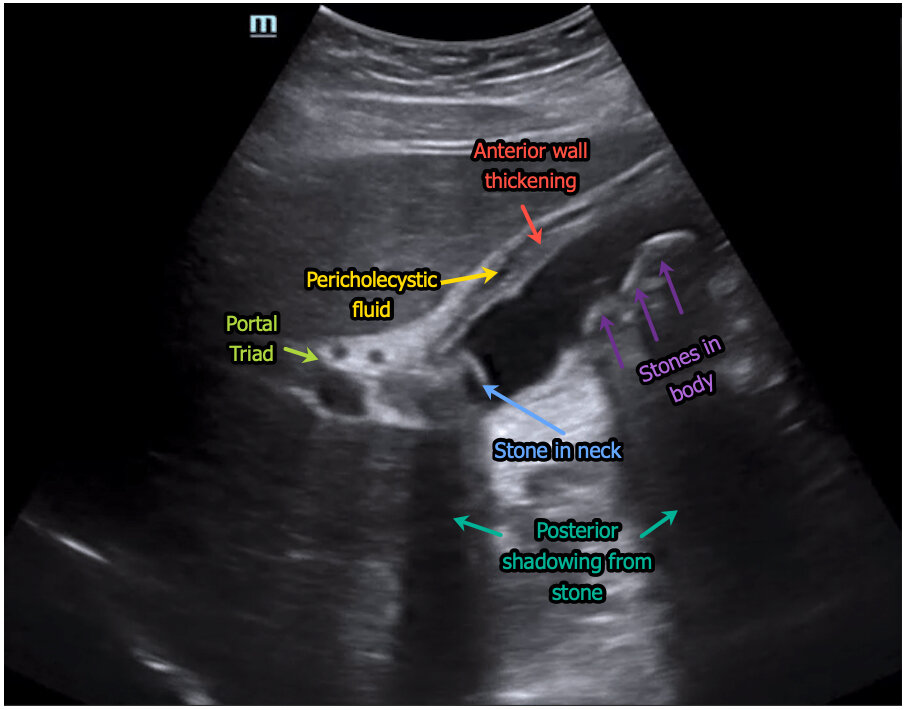
Long axis view — multiple gallstones including one in the neck (not the hyperechoic rim with clearly defined posterior shadowing. Wall thickening with pericholecystic fluid seen. The patient also had positive Sonographic Murphy’s sign (though obviously not depicted here).
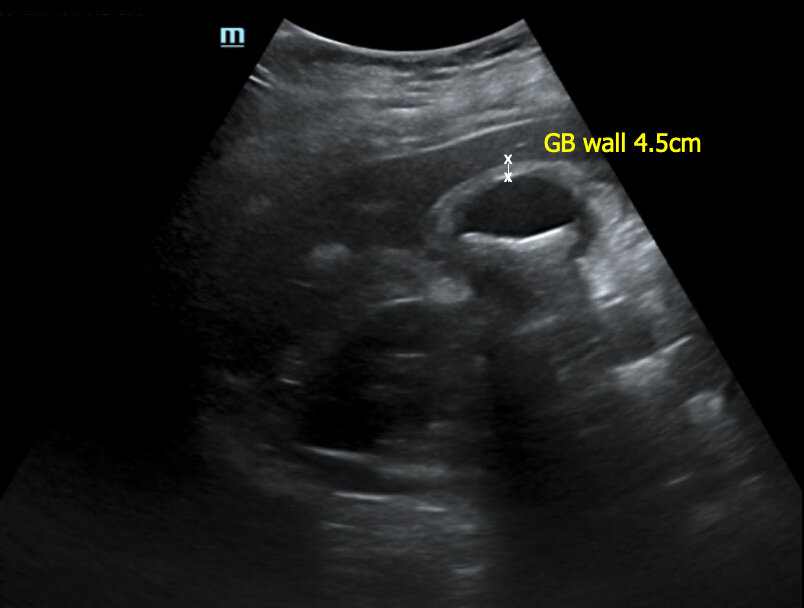
Thickened gallbladder wall 4.5 cm
Short axis view — can again see gallbladder wall thickening with echogenic stones and posterior shadowing.
A normal-appearing kidney also visualized.
CBD dilation, measuring 8mm
POCUS findings consistent with cholecystitis. CBD dilation also noted.
Case continued: Labs were significant for leukocytosis (surprisingly had normal LFTs/bili). No blood or infx in urine. She was given zosyn, kept NPO, and acute care surgery was consulted. They requested the "formal"/radiology-performed ultrasound, which was consistent with POCUS findings. She was admitted to surgery and added on to the OR schedule the next morning. Diagnosis confirmed in the OR. She was discharged the following day.
Biliary POCUS
Brief Background
Biliary disease is the 3rd most common cause of acute abdominal pain in the ED [1]
Physical examination and laboratory evaluation are poorly sensitive and specific for this diagnosis [2]
Radiology-performed RUQ ultrasound is traditionally the diagnostic test of choice to evaluate for biliary pathology but takes time and is not always readily available. As a result, biliary POCUS has become more popular and utilized by emergency physicians in recent years.
Clinical Questions
Are gallstones present?
Are there signs of cholecystitis?
Also, is CBD dilated? (suggestive of choledocholithiasis)
Technique
Curvilinear (or phased array) probe
Patient in supine position, knees flexed if possible to relax abdominal muscles. Left lateral decubitus or upright positioning often helps optimize imaging.
Locate the gallbladder. Its location various from one patient to another
Anterior approach: Place probe in epigastrium in longitudinal orientation. Identify the aorta. Slide toward patient right, moving along the costal margin — first you’ll see the IVC then the next fluid-filled structure will be the gallbladder. This order (aorta-IVC-gallbladder) is consistent.
Lateral approach: probe in mid-axillary line (RUQ FAST view). Locate the hepatorenal interface and slowly slide/fan the probe anteriorly
Intercostal approach: probe in midclavicular line, moving up and down rib spaces and medial and lateral; may need phased array probe as its smaller and will better fit between rib spaces
Look for exclamation mark (gallbladder in its long axis + short axis of portal vein) and portal triad to confirm gallbladder. Can also apply Color Doppler to confirm its not a vessel.
One you find the gallbladder, rotate the probe so that you visualize it in its longitudinal orientation (which is usually not the same as long axis of the patient’s body) followed by its short axis. Fan all the way through, looking for findings discussed below.
Identify the CBD. Sits above (anterior to) the portal vein, has brighter walls, no flow with Color Doppler. Can visualize in its long or short axis. Measure inner wall to inner wall
What to Look For [3]
Gallstones -- especially in the neck as this is where they're most problematic
Sonographic Murphy's sign (maximal pain elicited when probe is pressing directly on the gallbladder)
**One of the most important sonographic signs of cholecystitis [4]
Wall thickening > 3mm (measure anterior wall)
Pericholecystic fluid
CBD dilation > 6mm (inner wall to inner wall)
Pearls & Pitfalls
Ways to optimize imaging:
Place patient in left lateral decubitus position to help move bowel out of the way
Deep inspiratory hold helps move the gallbladder inferiorly, away from the ribs
Always view in long and short axis and fan all the way through
Must visualize the neck (it’s an incomplete study if you don’t)
Measure the anterior wall, preferably in short axis as this is most accurate (may get false positive measurement in long axis)
May have diffuse/uniform wall thickening in post-prandial states, renal failure/cirrhosis, HIV, etc [5]
CBD dilation thought to increase in older age [6]
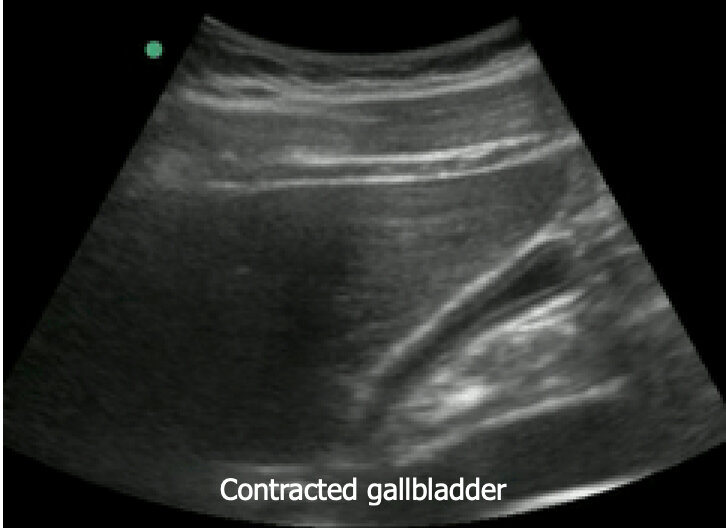
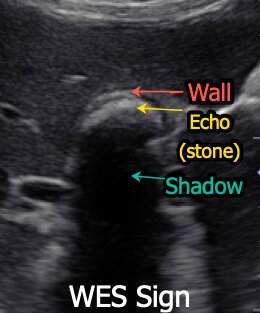
WES (wall echo shadow) sign — when gallbladder is contracted around multiple stones or single large stone, distorting normal appearance
Duodenum often mistaken for gallbladder w/ stone. Differentiate by lack of shadowing or dirty shadowing & presence of peristalsis)
Why Does This Matter?
Diagnostic accuracy (particularly sensitivity, specificity, NPV) of biliary POCUS is comparable to that of radiology-performed (“formal”) ultrasounds [7]
The presence of wall thickening, gallstones, and sonographic Murphy’s sign are highly specific in predicting need for OR [8]
Biliary POCUS associated with significantly shorter ED length-of-stay compared to that of patients undergoing radiology ultrasonography [8-9]
CBD dilation is suggestive of biliary obstruction but utility is controversial [10]
Take Home Message
Biliary POCUS is comparable to radiology-performed ultrasound with faster time to diagnosis and decreased ED length of stay. Don’t wait for the “formal” study to make the diagnosis!
POST BY: DR. ANNA HARNED, PGY1
FACULTY EDITING BY: DR. LAUREN MCCAFFERTY
References
Cervellin G, Mora R, Ticinesi A, et al. Epidemiology and outcomes of acute abdominal pain in a large urban Emergency Department: Retrospective analysis of 5,340 cases. Ann Transl Med. 2016;4(19):1-8.
Trowbridge RL, Rutkowski NK, Shojania KG. Does this patient have acute cholecystitis? JAMA. 2003;289:80-86. 3.
Noble V, Nelson B. Manual of Emergency Medicine and Critical Care Ultrasound, 2nd ed. Cambridge: Cambridge UP, 2011.
Noble VE, Liteplo AS, Nelson BP, Thomas SH. The impact of analgesia on the diagnostic accuracy of the sonographic Murphy's sign. Euro J Emerg Med. 2010 Apr 1;17(2):80-3
Perret RS, Sloop GD, Borne JA. Common bile duct measurements in an elderly population. Journal of ultrasound in medicine. 2000 Nov;19(11):727-30.
Runner GJ, Corwin MT, Siewert B, Eisenberg RL. Gallbladder wall thickening. Am J Roentgenol. 2014; 202(1): 202:W1–W12.
Summers SM, Scruggs W, Menchine MD, et al. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med. 2010;56(2):114-122.
Hilsden R, Leeper R, Koichopolos J, et al. Point-of-care biliary ultrasound in the emergency department (BUSED): Implications for surgical referral and emergency department wait times. Trauma Surg Acute Care Open. 2018;3(1):1-5.
Blaivas M, Harwood RA, Lambert MJ. Decreasing length of stay with emergency ultrasound examination of the gallbladder. Acad Emerg Med. 1999;6:1020-1023.
Lahham S, Becker BA, Gar A, et al. Utility of common bile duct measurement in ED point of care ultrasound: A prospective study. Am J Emerg Med. 2018; 36(6):962-966.