Intern Ultrasound of the Month: Posterior Vitreous Detachment
The Case
73 yo M with PMHx of HTN and thoracic aortic dissection presented for right eye “soreness”, primarily over medial canthus with associated watery discharge and injection. Stated it feels like there was a “film over his eye.” Does not wear contacts. Denied fever, chills, headache, significant change in visual acuity, flashes, floaters, pain with EOM, recent trauma.
Vital signs within normal limits, patient well-appearing.
Exam revealed: EOMI, visual fields intact to confrontation, 20/40 OD (20/40 OS), IOP 19 mmHg OD (17 mmHg OS), mild lnjection, medial pinguecula. No other significant findings
Point-of-care ultrasound performed and showed the following:
Wavy, hyperechoic membrane within the vitreous that swirls with extraocular movements and is not attached to the optic nerve. Findings suggestive of posterior vitreous detachment. A small amount of echogenic material also seen posteriorly, likely developing vitreous hemorrhage.
Case continued…
Ophthamology consulted, performed dilated eye exam and confirmed diagnoses. Patient discharged with close outpatient follow up & artificial tears for dry eyes.
Posterior Vitreous Detachment
Pathophysiology
Vitreous is the gel-like substance composed of collagen that fills the eye
Vitreous liquefies over time, referred to as syneresis
Some of the collagen can precipitate, creating “floaters”
As the vitreous continues to liquify, it contracts and can lead to separation of the vitreous from the retina
Typically benign course but complications may develop (see below); age-related PVD is an insidious asymptomatic chronic event
Complications include:
Retinal tear - develop in only 1.8% of patients with uncomplicated PVD
Retinal detachment
Vitreous hemorrhage
Optic hemorrhage
Clinical presentation
Flashes and floaters are common
Usually not sight-threatening
Diagnosis is usually by dilated eye exam; ultrasound good adjunct
Management/outcomes
Uncomplicated PVD is usually self-resolving and only requires education and reassurance
F/u with ophthalmology to ensure resolution
If symptoms persist or complications develop, surgery may be indicated
Ocular Ultrasound
Indications
Vision changes
Eye pain
Foreign body
Eye trauma
**Contraindication: concern for globe rupture
Technique
Linear probe (high frequency), probe marker to patient right
Cover eye with tegaderm ( remove air bubbles),
Apply a lot of gel & stabilize hand on pt’s face to control amount of pressure applied
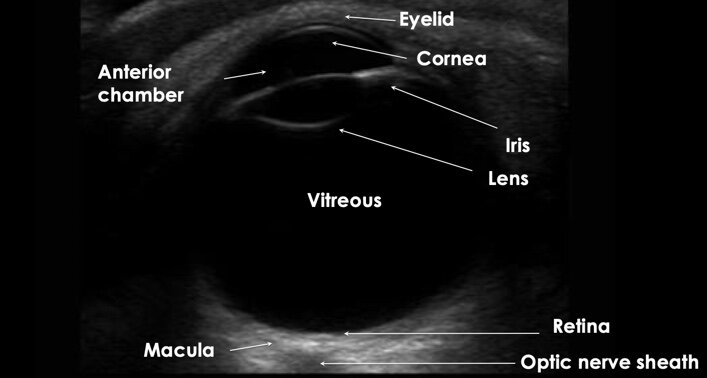
Identify structures of eye
Turn down the gain to evaluate optic nerve (& structures posteriorly)
Slowly increase gain to better visualize abnormalities within vitreous
Kinetic/dynamic exam: have patient look side to side
Vitreous detachment
Wavy, hyperechoic membrane within the vitreous that’s NOT attached to the optic nerve
Free floating & swirls with extraocular movement (washing machine sign)
May see vitreous hemorrhage — fluid collection of variable echogenicity in vitreous chamber that moves with kinetic exam
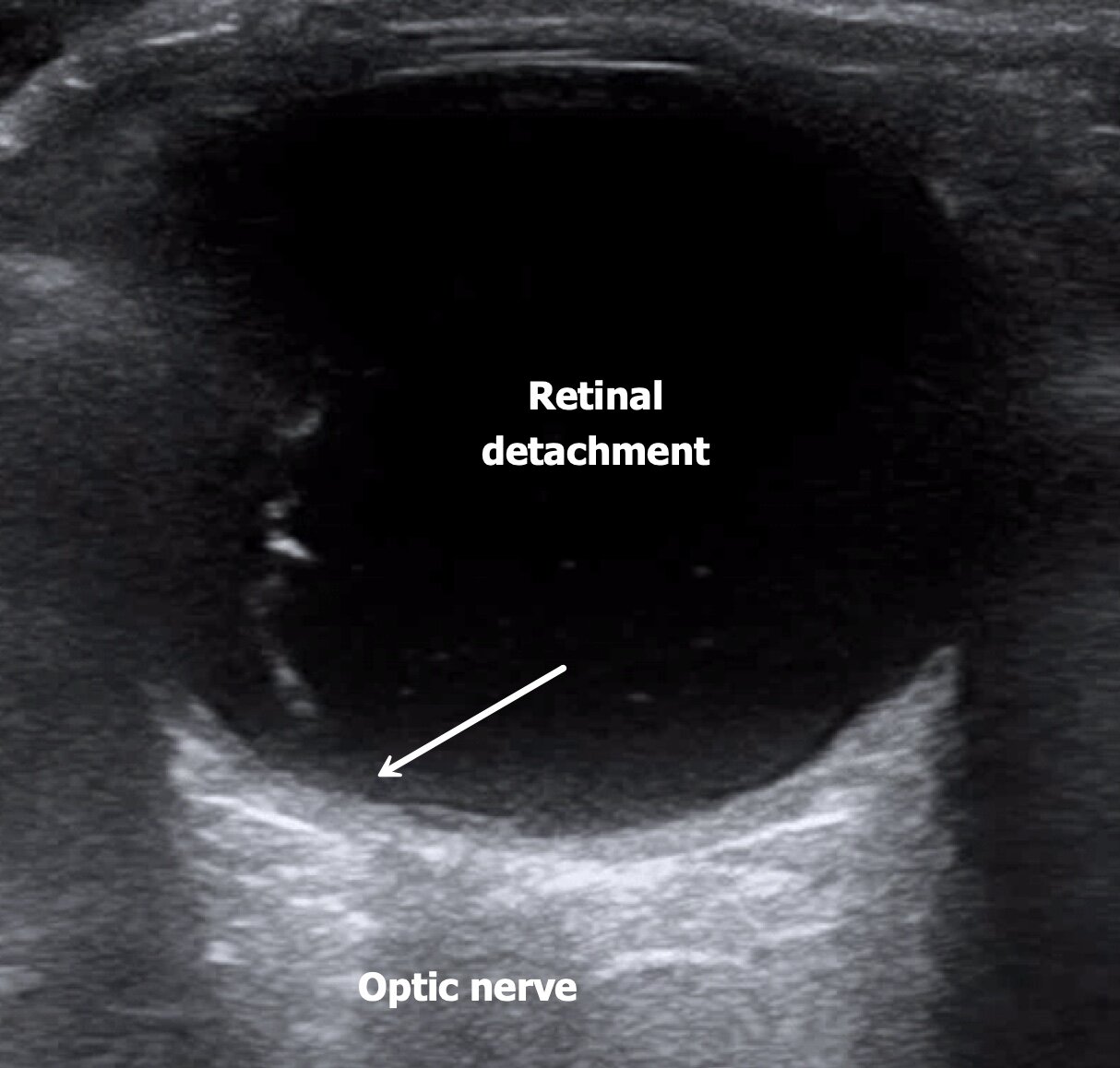
Compare to retinal detachment (ophthalmologic emergency) which extends from/is attached to the optic nerve (see below)
***Must visualize optic nerve to differentiate between the two
Vitreous Detachment
Retinal Detachment — Note how the hyperechoic membrane is tethered to /extends from the optic nerve & doesn’t cross midline
What’s the evidence?
Ultrasound hasn’t demonstrated the best accuracy for vitreous detachment or hemorrhage but relatively higher accuracy for retinal detachment, which is the ophthalmologic emergency (Lahham et al, 2019)
Overall, it’s a useful adjunct to ophtho exam and can be rapidly performed at the bedside
POST BY: DR. RAY JABOLA, PGY1
FACULTY EDITING BY: DR. LAUREN MCCAFFERTY
References
Johnson MW. Posterior Vitreous Detachment: Evolution and Complications of Its Early Stages. American Journal of Ophthalmology. 2010;149(3)
Lahham S, Shniter I, Thompson M, et al. Point-of-Care Ultrasonography in the Diagnosis of Retinal Detachment, Vitreous Hemorrhage, and Vitreous Detachment in the Emergency Department. JAMA Netw open. 2019;2(4):e192162.
Thepocusatlas.com
Uptodate.com
Vitreous Syneresis: An Impending Posterior Vitreous Detachment (PVD). https://webeye.ophth.uiowa.edu/eyeforum/cases/196-PVD.htm. Accessed December 11, 2019.
5minsono.com