Tox in The Land: Tricyclic Antidepressants
Amitriptyline
What is a tricyclic antidepressant?
Three ring structure with amine group attached
3 benzene ring core (hence the tricyclic!)
Secondary or tertiary amines
Secondary –greater blockage of NE reuptake
Tertiary—greater blockage of Serotonin reuptake
FDA approved first TCA for treatment of MDD in 1959
“Tofranil” Imipramine was first drug approved in this class
Derived from promethazine by substituting sulfur bridge for an ethylene bridge
Originally created for use as an antipsychotic by the Geigy Chemical Corporation
Fell out of favor due to their side effects and development of safer options-ie, SSRI
What else is it used for?
Adjunct analgesics in for treatment of neuropathic pain
Obsessive-compulsive disorder (Clomipramine)
Migraine prophylaxis (Doxepin and Amitriptyline)
Fibromyalgia (second line treatment)
Insomnia, chronic pain, anxiety
Common TCAs out in the wild
Amitriptyline
Nortriptyline
Clomipramine
Doxepin
Imipramine
Trimipramine
Desipramine
Pharmacokinetics
Rapidly absorbed after oral ingestion, high bioavailability
Therapeutic plasma concentration level 50-3000ng ml, reached in 2-8hrs
Half life ranges from 7-58 hours
Metabolized by CYP2D6 in Liver
Demethylation
Hydroxylation
Glucuronidation
Excreted through urine
Mechanism(s) of Action
TCAs have a ton of MOA leading to a variety of uses and presentations when toxicity develops
Inhibits reuptake of Serotonin and NE at presynaptic membrane
Competitive antagonist on postsynaptic membranes
Alpha 1
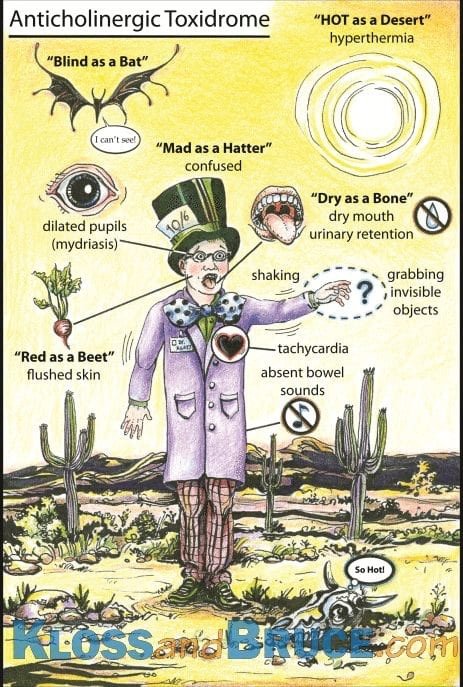
Anticholinergic
Muscarinic
Histamine
Sodium channel blocker
Potassium efflux blockade
GABA A antagonism
Clinical Effects
Well, with all of those mechanisms it’s not surprising that TCAs fell out of favor.
However, they can be very effective for a lot of patients when used appropriately.
When toxicity develops, patients can present with predominantly cardiac and neurologic effects
CNS Effects
Lowers seizure threshold
GABA A antagonism leading to increase CNS activity
Opposite end of spectrum
Mental status depression
Delirium
Coma
Alpha 1-adrenergic blockade
Na channel blockade
Anticholinergic
H1 blockade
Antimuscarinic
Cardiac Effects
Sodium channel blockade and K efflux blockade can lead to some of the more serious cardiac effects seen
The most common EKG change is sinus tachycardia
RBBB, RAD, terminal R wave in aVR
When the widening continues…
QRS prolongation can lead to CV collapse
QTc prolongation, especially in conjunction with a slowing HR can lead to TdP
Management
Benzos and supportive care? Why, of course…with some extras
Neurologic symptom management
ABCs
Benzos as needed for seizures and agitation
Intubation can be needed at times due to profound CNS depression or due to elevated sedation needs
Physostigmine
Controversial due to case series showing development of asystole in patients given physo after TCA overdoses…stay wary…stay away from physo. + TCA combination
Managing cardiac effects
Sodium bicarb, sodium bicarb, sodium bicarb
Dose to narrowing of QRS
Overcomes Na blockade, conformational change can knock TCA off receptors
Hypertonic saline
K repletion and Mg for QTc management
Lipids…only if crashing
Vasopressors/Inotropes as needed for refractory hypotension
ECMO…possible but not usually
Tachycardia is protective against TdP, don’t focus on the rate, focus on the
intervals
Goals of Treatment with Bicarb
Narrow that QRS
QRS <100ms
Na 145-155
pH 7.45-7.55
K>4
Mg>2
Improved perfusion
Who is going to get sick?
Cardiac effects can be a marker for toxicity
Previous studies have shown that
QRS<100 -no seizures or ventricular dysrhythmias
QRS<160 -seizures seen, no ventricular dysthymias
QRS>160 –seizures and ventricular dysthymias
What does this mean…get your EKGs!
Dispo from the Emergency Department
Asymptomatic patients with normal vitals and EKG can be cleared after a 6-hour observation period (from time of overdose)
Symptomatic…admit :)
Fun fact…the 6-hour obs window commonly used in ED observation windows came from TCA overdoses and their prevalence
POST BY: DR. WESLEY GALLAHER (R3)
FACULTY EDITING BY: DR. LAUREN PORTER
References
Body R. (GEMNet): guideline for the management of tricyclicantidepressant overdose. EMJ. 2001; 28:347-368. doi:10.1136/emj.2010.091553
Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1-21. doi:10.1037/a0038550
Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. EMJ. 2001;18:236-241.
Moraczewski J, Aedma KK. Tricyclic Antidepressants. [Updated 2020 Dec 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557791/
Pereira V, Hiroaki-Sato V. A brief history of antidepressant drug development: From tricyclics to beyond ketamine. Acta Neuropsychiatrica. 2108; 30(6), 307-322. doi:10.1017/neu.2017.39 Guidelines in Emergency Medicine Network
Liebelt EL, Ulrich A, Francis PD, Woolf A. Serial electrocardiogram changes in acute tricyclic antidepressant overdoses. Crit Care Med. 1997; 25(10):1721-6. doi: 10.1097/00003246-199710000-00024. PMID: 9377889.
Kloss B. Anticholinergic toxidrome. LITFL. Published April 21, 2019. Accessed July 2022. <https://litfl.com/anticholinergic-toxidrome/>
Burns E, Buttner R. Tricyclic Overdose. LITFL. Published August 1, 2018. Accessed July 2022. <https://litfl.com/tricyclic-overdose-sodium-channel-blocker-toxicity/>